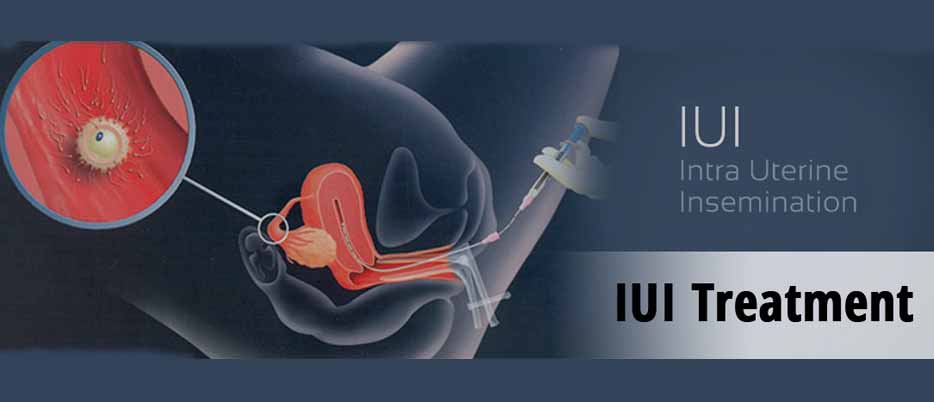
Intrauterine Insemination (IUI) is a fertility treatment that involves placing sperm directly into a woman’s uterus to increase the chances of conception. While this procedure has helped many couples overcome infertility, there are several misconceptions about IUI that can lead to confusion or hesitation for those considering it. Addressing these misconceptions can provide a clearer understanding of the procedure and its benefits.
Misconception: IUI is a “last resort” fertility treatment
One of the most common misconceptions is that IUI is only used when all other fertility treatments have failed. In reality, IUI is often one of the first treatments recommended for couples struggling to conceive, particularly if the cause of infertility is unclear or linked to mild issues like low sperm count or cervical mucus problems. It’s less invasive and less costly compared to treatments like In Vitro Fertilization (IVF), making it a starting point for many couples. It can also be paired with ovulation-stimulating medications to improve success rates.
Misconception: IUI guarantees pregnancy
Although IUI increases the chances of pregnancy, it’s important to recognize that it does not guarantee success. The success rates for IUI vary based on several factors, including the woman’s age, the quality of the sperm, and whether fertility medications are used. On average, the success rate for IUI can range from 10% to 20% per cycle. While this makes it a valuable option for couples facing infertility, it is not a guaranteed solution. Many couples require multiple IUI cycles before achieving pregnancy.
Misconception: IUI is painful
Some people worry that IUI is a painful procedure, which can create unnecessary anxiety. However, IUI is typically described as a simple and relatively painless process. The procedure is similar to a Pap smear in terms of discomfort, involving the insertion of a catheter into the uterus to deposit sperm. Most women experience only mild cramping or discomfort during or after the procedure, which usually subsides quickly. Pain associated with IUI is generally minimal and temporary.
Misconception: IUI is only for couples with female infertility issues
Another common myth is that IUI is only used when the woman is facing fertility issues, such as ovulation problems or unexplained infertility. However, IUI can also be effective for men with mild to moderate male infertility issues, such as low sperm count or motility. By placing sperm directly into the uterus, IUI helps the sperm bypass barriers like the cervix, increasing the likelihood of sperm reaching the egg. It’s also used for single women or same-sex couples who are using donor sperm.
Misconception: IUI is ineffective compared to IVF
While IVF is often seen as a more advanced fertility treatment, IUI can still be effective depending on the situation. For couples with unexplained infertility, mild male infertility, or certain female fertility issues, IUI can offer a simpler and more affordable option. IVF is more invasive and expensive, and while it offers higher success rates, many couples find success with IUI before moving to IVF. It’s important to consult with a fertility specialist to determine the most appropriate treatment based on individual circumstances.
Misconception: Age doesn’t affect IUI success rates
Some believe that age has no impact on IUI outcomes, but this is not true. Just like with natural conception, a woman’s age significantly influences the success of IUI. Women under 35 tend to have higher success rates, while those over 40 may experience lower success rates due to a decline in egg quality and quantity. Although IUI can be effective for older women, it is often recommended to try more advanced treatments like IVF as a woman’s age increases.
Misconception: IUI always requires fertility drugs
While fertility drugs can be used in conjunction with IUI to stimulate ovulation and increase the chances of pregnancy, they are not always necessary. Some women have regular ovulation and do not need medication to increase egg production. In such cases, natural cycle IUI, where the woman’s natural ovulation is monitored, can be performed without medication. The decision to use fertility drugs depends on individual fertility challenges and the doctor’s recommendations.
Conclusion
Intrauterine Insemination (IUI) is a valuable fertility treatment for many couples, but misconceptions about the procedure can create unnecessary fears or misunderstandings. By addressing these myths, individuals and couples can approach IUI with a clearer understanding of its potential benefits, limitations, and how it fits into their fertility journey. Consulting with a fertility specialist is key to making informed decisions and finding the right path to parenthood.