One of the most well-known assisted reproductive technologies (ART) used to assist infertile couples is in vitro fertilization treatment. For those who are not able to conceive naturally, this treatment entails a series of surgical operations that fertilize an egg outside the body. IVF has revolutionized the field of reproductive health and given hope to countless single people and couples hoping to expand their family.
What is IVF?
The term “in vitro” means “in glass,” referring to the laboratory environment where fertilization occurs. In IVF, eggs are retrieved from a woman’s ovaries and fertilized by sperm in a controlled setting. Once fertilized, the resulting embryos are monitored, and one or more may be transferred into the woman’s uterus in hopes of achieving pregnancy.
IVF is often chosen by couples after other fertility treatments, such as medications or intrauterine insemination (IUI), have failed. However, it’s also a first-line treatment for certain conditions like blocked fallopian tubes, severe male factor infertility, or when genetic testing of embryos is necessary.
Who Benefits from IVF?
IVF treatment is beneficial for a wide range of fertility issues. Some of the most common reasons for pursuing IVF include:
Blocked or damaged fallopian tubes: For women with blocked or damaged tubes, IVF bypasses this issue by retrieving eggs directly from the ovaries.
Male factor infertility: Men with low sperm count or poor sperm motility may still achieve fertilization through IVF, particularly with the use of Intracytoplasmic Sperm Injection (ICSI), a process that injects a single sperm directly into an egg.
Endometriosis: This condition, where tissue similar to the lining of the uterus grows outside of it, can cause fertility issues that may be resolved with IVF.
Unexplained infertility: For couples where no specific reason for infertility is found, IVF offers a structured and often effective way to conceive.
Genetic concerns: IVF allows for preimplantation genetic testing (PGT), where embryos are screened for genetic disorders before being transferred into the uterus, helping to reduce the risk of passing on inherited conditions.
The IVF Process
In vitro fertilization treatment is a multi-step process that generally takes several weeks. It involves the following key stages:
Ovarian stimulation: To begin, the woman is prescribed hormone injections to stimulate her ovaries to produce multiple eggs. This is monitored through blood tests and ultrasounds to track the growth of follicles, where eggs develop.
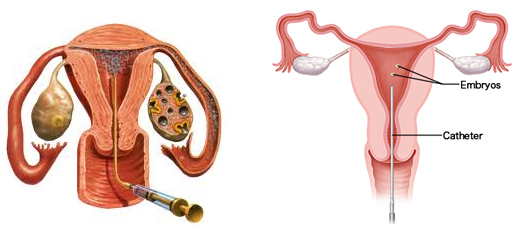
Egg retrieval: Once the eggs are mature, they are retrieved through a minor surgical procedure called follicular aspiration, which involves inserting a needle through the vaginal wall and into the ovaries to collect the eggs.
Fertilization: The retrieved eggs are combined with sperm in a laboratory. In some cases, ICSI may be used to directly inject a sperm cell into an egg, ensuring fertilization.
Embryo development: Fertilized eggs, now called embryos, are kept in an incubator where they grow for about five days. The best-quality embryos are selected for transfer.
Embryo transfer: Typically, one or two embryos are transferred into the woman’s uterus through a thin catheter. The goal is for one of these embryos to implant into the uterine lining and result in a pregnancy.
Pregnancy test: About two weeks after the embryo transfer, a blood test is performed to determine if the treatment was successful and the woman is pregnant.
Success Rates and Considerations
The success rates of IVF depend on a variety of factors, including the woman’s age, fertility issues, and the quality of the embryos. On average, women under 35 have a 40-50% chance of success per cycle, while those over 40 see reduced success rates. It’s also important to note that IVF can require multiple cycles to achieve a successful pregnancy, which can be physically, emotionally, and financially taxing.
In addition to success rates, potential risks associated with IVF include ovarian hyperstimulation syndrome (OHSS), where the ovaries overreact to fertility drugs, multiple pregnancies (when more than one embryo implants), and the emotional impact of potential treatment failures.
Advances in IVF Technology
As reproductive technology evolves, so do IVF techniques. Innovations such as time-lapse imaging allow embryologists to monitor embryo development more precisely, improving selection for transfer. Additionally, advancements in freezing technologies, like vitrification, allow for the successful storage of eggs and embryos for future use without compromising their viability.
Conclusion
In vitro fertilization (IVF) offers a path to parenthood for many who face infertility challenges. While the process is complex and sometimes emotionally demanding, the advancements in reproductive medicine continue to improve the chances of success for individuals and couples worldwide. Whether due to blocked fallopian tubes, male infertility, or genetic concerns, IVF remains one of the most promising fertility treatments available today, providing hope to those eager to grow their families.